Issues in diagnosing glaucoma
Medicine is an art and not a science. Although the diagnosis of glaucoma is based upon years of scientific investigation and research, the diagnosis of glaucoma involves a great amount of diagnostic skill. It is at times difficult to diagnose a disease that has no symptoms until it produces blindness. And because symptoms in the early stages of glaucoma are uncommon it is uncommon for people to present themselves for a thorough eye examination until too late.
While looking for manifestations of the disease in the early stages, several confounding variables exist. Predominant among these is that normal in medicine is never an absolute value but is represented by a range. Can this apparently suspicious looking factor actually be a part of the wide variation of normal?
Glaucoma is truly present only if damage is noted in the optic nerve and or nerve fibre layer (structural damage). The level of eye pressure usually does not make that much difference as does the appearance and function of the optic nerve. However, the risk of glaucoma can greatly increase if the eye pressure gets high. In these situations, treatment to lower the eye pressure may need to be taken, despite the fact that there might still not be any damage present. In other words treatment may need to be started when the risk of developing glaucoma and loosing vision is higher than the risk of the treatment itself.
What Risk Factors Predict The Likelihood of Getting Glaucoma?
We do not know why some people get glaucoma and some don’t. But we do know that glaucoma is a dangerous eye disease because often there are no symptoms until serious damage has occurred. Since damage from glaucoma is irreversible, one wants to identify factors (risk factors) which increase the possibility of having / developing glaucoma.
Established risk factors for glaucoma include:-
- Age over 40 years of age
- Glaucoma in the family
- Have diabetes/ thyroid disease / hypertension
- Have received steroid containing preparations : tablets/ drops/ ointments/ puffs/ injections
- See rainbow coloured rings around bright light
- Rapid change of glasses
- Taking medication for sleep / anxiety / depression / asthma/ parkinsonism / prostate
- Injury to the face /eye
- Myopia
- Have headaches
Testing for Glaucoma
To detect glaucoma one usually needs a complete eye examination with an emphasis on:-
Tonometry, Ophthalmoscopy, Perimetry and Gonioscopy (TOP-G test)
- Tonometry is the method by which the pressure within the eye is measured. Ideally it needs to be done with an instrument called the tonometer which uses blue light.
For most normal people eye pressures are usually within 11- 21 mmHg, but then the figure of 21 is not sacrosanct. It is possible to have glaucoma induced damage to the optic nerve even when the eye pressure is 15mmHg (in the normal range) just as an eye pressure of 25 mmHg may be associated with no damage to the nerve. This may sound ambiguous but the point to make is that the diagnosis of glaucoma is not dependent on the eye pressure alone and it is important that other parameters are also looked at also.
Procedure: To measure the eye pressure, an eye drop, which might sting for a few seconds, is placed on the eye. This numbs the eye. A probe is next placed on the eye which measures the pressure within. The pressure inside the eye is related to how much force is needed to indent the cornea just a little bit. This process does not hurt and only takes a few seconds.
Frequency:The eye pressure with the blue light needs to be checked at every visit.
- Ophthalmoscopy is the technique by which an instrument is used to look into the status of the optic nerve. It needs to be done typically for everyone who wants a complete eye examination. Those with glaucoma would need to get it done more frequently than others.
The optic nerve is not a “single” nerve, but a collection of approximately 1,000,0000 (one million) nerve fibers arranged like the fine wires within a cable. Normally, each one of us looses 5,000 fibers a year through the process of aging, normally. The optic nerve is the only living nerve in the human body which can be seen without making an incision. The optic nerve is also the structure that transfers the image seen by the eye as an electrical impulse to the brain which reconstructs the image and then sends a command to the eye again as an electrical impulse with instructions to follow up on the object in question.
When these nerve fibers are injured, as in glaucoma, it causes loss of vision. Damage to the optic nerve is permanent and cannot be reversed. Also once some damage occurs then it is easier for further damage to develop relatively easily. Once the optic nerve is totally destroyed, an eye will not be able to perceive light at all.
Procedure for examining the optic nerve. The optic nerve is located in the back of the eye, behind the pupil. Normally if one shines a light on the pupil, the pupil constricts making it extremely difficult, if not impossible to examine the optic nerve’s structure. One therefore needs to put dilating drops in the eye to negate the pupil. These drops temporarily stretch the pupil’s muscles so that the pupil, or the window to the back of the optic nerve, will stay open while examining the nerve. The effect of these drops usually lasts for a few hours. While the effect of the drops is present, lights will appear brighter and reading will be difficult.
Examining the way the optic nerve looks is very important to diagnose glaucoma. Detecting glaucoma in the early stages is sometimes possible only by looking at the optic nerve and the way it functions. This helps to decide whether there is glaucoma and the extent to which the optic nerve is damaged. Repeated examinations allow us to detect worsening over time and modify treatment to prevent further damage to the optic nerve.
Since examining the optic nerve is essential, not just for the diagnosis of glaucoma, but also to assess possible worsening with time, it is important to document changes with the help of photographs serially over time. These are not X-Rays, but just digital pictures which are printed /stored. Despite how bright the flashlight appears, there is no risk from the process of taking photographs of the optic nerve.
Frequency:Ideally an optic disc examination needs to be scheduled every six months to once a year depending on the severity of the glaucoma.
- Perimetry : Visual field Examination (VFA) / Automated Perimetry:
The field of vision is the part of space we can see at any given moment. This can be easily demonstrated.Please try closing your left eye and circle the right eye with the index finger and thumb kept close to the eye. All that we can see now is through the circle formed by the index finger and thumb kept close to the eye and represents the field of vision for this eye.
Now if one takes this circle away from the eye, one can see within the circle and outside the circle. In glaucoma one loses this ability to see outside the circle and with gradual worsening, the circle of vision gets reduced till no vision is left.
Assessing the visual field is actually trying to measure the function of the optic nerve. This test measures the side vision. This is important because the loss of vision begins on the sides and is not noticed by patients until the glaucoma has become very advanced. Since the damage in glaucoma is irreversible, the aim of treatment is stopping the damage before it gets advanced, or if one already has an advanced damage, then the aim is to prevent further worsening.
In glaucoma the fields are tested with the automated perimeter. This also helps to detect and document change over time. This machine-based test is designed to show flashes of light of varying intensity such that if a point is normal, one will be able to perceive the light. However, if it is truly normal then dim light will also be seen and conversely if a point is diseased then only bright light will be seen. Based on the responses to flashes of light of varying intensity, one’s responses are compared with a group of normal in the same age group and a display representing the deviation from normal is prepared.
It’s important to remember that one is not likely to see more than 50% of the light that is shown. This holds good even for those who are normal because the intensity of light is always being varied.
Nobody likes visual field testing because it can be frustrating and boring. But with proper guidance and support it is usually possible to do a perimetry well even in the first time. Remember, if one is having trouble with the testing, or is tired, ask the perimetrist to stop and re explain the test once more or to give you a rest break.
If the glaucoma worsens, visual field defects get larger and can the leave patient with a “tunnel vision” before blinding them. This can be very dangerous, as one would, not be able to see things on the side. It can cause a person to bump into objects or stumble and fall.
Frequency: Perimetry is a test which helps to detect worsening over time and hence needs to be repeated periodically. Depending on the severity of damage, perimetry may need to be done as early as once in three months (advanced glaucomas), once in six months for moderate to early glaucomas and once a year in those suspected to have glaucoma.
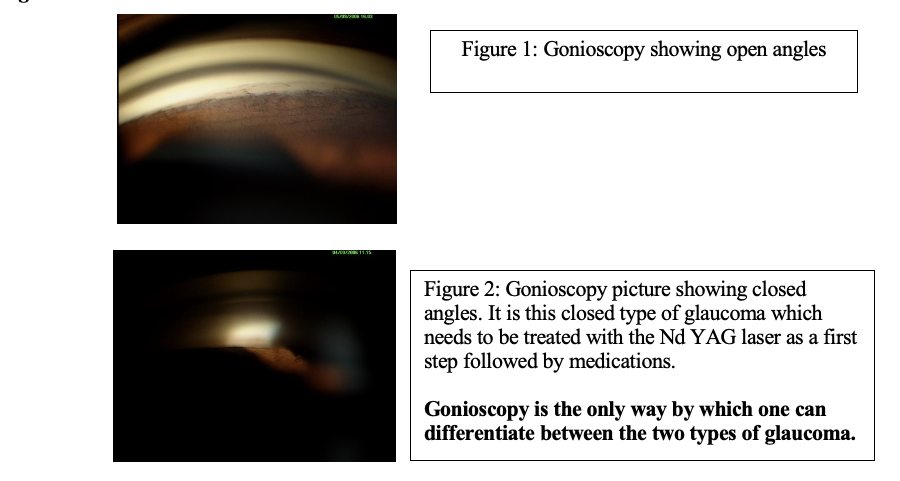
- Gonioscopy
The kind of glaucoma one has is determined by a very special contact lens called gonioscope which contains an angled mirror and helps to identify the type of glaucoma. It is important to know the kind of glaucoma one has as different types of glaucomas are treated differently.
In the open type treatment is usually started with eye drops used alone or in combination. And if that cannot lower the eye pressure to the desired level a glaucoma surgery would be required.
The closed type of glaucoma needs to be treated with the Nd YAG laser as a first step. If required, medication in the form of drops may also be required (depending on the severity). When these don’t work a glaucoma surgery may need to be considered.
Gonioscopy is the only way by which one can differentiate between the two types of glaucoma.
Procedure: After the eye has been numbed, a special contact lens is placed on the eye to look around the corners to help see things that normally could not be seen. This is not the same type of contact lens which helps you see, but it helps us to see into the eye. It does NOT permanently stay on your eye. This type of contact lens helps determine whether, or not, you have an open-angle glaucoma.
It is very important to make sure that the correct diagnosis is made ensuring that the correct treatment is instituted early on. This contact lens stays on the eye for a matter of a minute or so. One will not even realize when the lens has been placed or removed from the eye.
Frequency: At the first visit and then once a year. At times it may need to be done more frequently.
Role of Newer Imaging Devices
Stereoscopic photography, the current gold standard for assessing optic nerve change allows the eye doctor to document change over time. Color photography with a 15 degree field gives optimal magnification. Interpretation may be subjective. Reputed clinical trials and studies have used qualitative evaluation of stereoscopic optic disc photographs as an outcome measure indicating an acceptance of stereoscopic optic disc photography as a valid tool for detection and monitoring of glaucoma.
The last few years have seen the emergence of a host of newer instruments – optic nerve imagers and retinal fiber layer analyzers, capable of providing objective and reproducible information about the optic disc and retinal nerve fiber. This information provided is usually beyond what’s obtainable from a clinical examination and is useful for diagnosing glaucoma and also to assess deterioration over time
Optical Coherence Tomograph (OCT ) provides for high resolution cross sectional imaging of the human retina and nerve fiber layer. The nerve fiber layer measurements are automated and displayed by quadrants, clock hour and an overall mean. OCT assessment of peripapillary retinal nerve fiber layer thickness has been reported to differentiate normal from glaucomatous eyes.
Confocal Scanning Laser Ophthalmoscopy: The Heidelberg Retinal Tomograph (HRT), is a scanning laser ophthalmoscope utilizing confocal scanning diode technology to provide topographic measurements of the optic disc and peripapillary retina. In a confocal system a laser beam is scanned across the retina and reflected back to a detector through a system of two conjugate pinholes, one in front of the laser source and the other in front of the detector. Through the use of algorithms that account for eyes movements, each scanned image in the series can be aligned. The HRT uses a fixed 150 field of view with 384 x 384 pixels per image plane and is more friendly clinically with automated fine focus and quality control checks to ensure image quality.
HRT is most helpful in evaluating the optic nerve for change, for evaluating glaucomatous progression. Measurements of optic disc stereometric parameters by HRT are highly reproducible. Research suggests that there may be a subset of patients with ocular hypertension in whom sequential follow-up with HRT can reveal optic nerve head changes which predate development of glaucomatous field changes. Advantages of the HRT include rapid image acquisition time, lack of need for pupillary dilation and images can be obtained through contact lenses or refractive errors can be compensated for prior to scanning.
Conclusion: Role of Newer Imaging Devices
1) Role in diagnosis of glaucoma: The parameters of IOP and visual field assessment can miss the diagnosis of glaucoma, especially in the early stages. In fact, upto 40% of the ganglion cells must be lost for a detectable loss on automated perimetry. Because optic nerve damage is irreversible early detection is crucial. The objective of imaging of the optic nerve head and retinal nerve fiber layer is to precisely quantify structural measurements. A comparison with normal allows early detection of glaucoma.
A word of caution: Categorizing patients to have glaucoma or no glaucoma by measurements obtained from imaging devices is not the same as diagnosis. The diagnosis of glaucoma requires the integration of available information obtained by clinical examination of the optic nerve and retinal nerve fiber layer, visual field status, gonioscopy and possible risk factors .
At this point of time The Association of International Glaucoma Societies (AIGS) does not acknowledge the role of any newer imaging modalities in the diagnosis of glaucoma.
2) Role in assessing deterioration in glaucoma: Comparison of these optic nerve and retinal nerve fiber layer changes over time helps to assess possible deterioration. Currently the confocal scanning laser ophthalmoscope Heidelberg Retinal Tomograph, is most sensitive to assess progressive changes from glaucoma in the optic nerve head. It has been shown in peer review literature that the HRT can detect possible worsening in 75% of glaucomatous population a year and a half before conventional tests can pick up the same. This makes it a very useful technology in glaucoma.

